*This content has been reviewed by Dr. Donna Vine (Agriculture, Food and Nutritional Sciences, University of Alberta); Last updated January 2025
Type 2 Diabetes occurs when the body cannot use insulin properly or does not make enough insulin to control blood glucose levels.
- Risk Factors for Type 2 Diabetes. Diabetes Canada identifies major risk factors for type 2 diabetes, including age, family history, ethnicity, obesity, high blood pressure, and lifestyle factors such as smoking, unhealthy diet, and physical inactivity.
- Added Sugars and Type 2 Diabetes. Recent evidence from systematic reviews and meta-analyses shows that consuming sugars does not increase risk of type 2 diabetes. Instead, any association between sugars and type 2 diabetes is mediated by sugars’ contribution to total calorie intake above energy needs, which can lead to weight gain and contribute to obesity, a major risk factor for type 2 diabetes. Research also suggests that high intakes of sugars-sweetened beverages in excess of energy needs may increase risk of type 2 diabetes, however this may be associated with an overall unhealthy diet and lifestyle pattern.
- Sugars and Carbohydrates Recommendations for Individuals with Type 2 Diabetes. Diabetes Canada Clinical Practice Guidelines (2018) state that individuals with Type 2 Diabetes may substitute added sugars for other carbohydrates as part of their meals up to a maximum of 10% of total daily energy intake, and choose low glycemic index foods more often.
Risk Factors for Type 2 Diabetes
There are many different factors that increase your risk of developing type 2 diabetes (1, 2). Diabetes Canada identifies the following risk factors for type 2 diabetes:
- Age – Being 40 years or over
- Genetics – e.g. Having a first-degree relative with type 2 diabetes
- Ethnicity - Being of African, Arab, Asian, Hispanic, Indigenous, or South Asian descent
- Weight - Having obesity/overweight, especially excess abdominal weight
- Health complications – e.g. having a history of prediabetes or gestational diabetes, high blood pressure, or high cholesterol and triglycerides in the blood
- Certain diagnosed conditions – e.g. having polycystic ovary syndrome, psychiatric disorders (schizophrenia, depression, bipolar disorder), or obstructive sleep apnea
- Other – Having darkened patches of skin, called acanthosis nigricans
Maintaining a healthy body weight is encouraged. Diabetes Clinical Practice Guidelines state that the most important risk factor for type 2 diabetes is having excess body fat (obesity), which can result from consistently consuming calories above energy needs (2).
Managing Diet for Type 2 Diabetes
The World Health Organization recommends that “a healthy diet, regular physical activity, and maintaining a normal body weight are ways to prevent or delay the onset of type 2 diabetes” (3).
Diabetes Canada suggests several healthy eating tips (4):
- Eating more vegetables.
- Choosing lean animal proteins such as fish, chicken, lean cuts of meat, low-fat cheese, eggs, and plant protein alternatives such as beans, lentils and peas.
- Using plant oils such as olive and canola in food preparation and dressings and consuming nuts more frequently.
- Eating smaller portions of grains and starches, including rice, potato, pasta, cereals, breads, or corn.
Added Sugars and Type 2 Diabetes
A number of international health agencies have reviewed the science on sugars and type 2 diabetes. For example,
- European Food Safety Authority – Found that there is no consistent evidence that consuming free sugars increases the risk of type 2 diabetes when calorie intake remains the same. The body's response to dietary sugars can differ greatly based on a person's metabolic profile. However, there was evidence with high certainty to suggest a positive relationship between drinking high amounts of SSBs (resulting in an increase in total energy intake) and risk of type 2 diabetes (5).
Recent evidence from systematic reviews and meta-analyses shows that consuming sugars does not increase risk of type 2 diabetes (6-8). Instead, any association between sugars and type 2 diabetes is mediated by sugars’ contribution to total calorie intake above energy needs, which can then lead to weight gain (see diagram below).
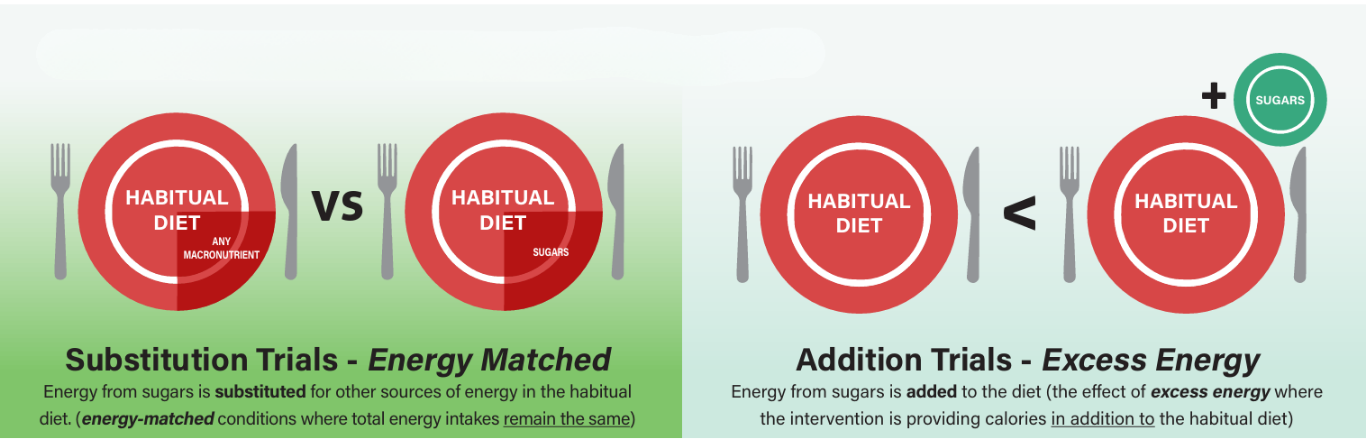
- In studies where sugars were substituted for other sources of carbohydrates such as refined starches and provided the same amount of total calories in the diet, there were no differences in body weight (7).
- When sugars were consumed on top of the regular diet and provided excess calories, weight gain did occur, which can contribute to an increased risk of type 2 diabetes.
Food Sources of Sugars and Type 2 Diabetes
The types of foods and drinks that contain sugars are important when it comes to potential contribution to diabetes risk (9-11).
- Research suggests that high intakes of sugars-sweetened beverages in excess of energy needs may increase the risk of type 2 diabetes.
- Other food sources of sugars (e.g. yogurt, fruit, whole grain breakfast cereals, and chocolate) have been associated with lower risk of type 2 diabetes.
Drinking large amounts of sweetened beverages is often linked to diet and lifestyle patterns that also include consuming calories and fat above energy needs, high amounts of sodium, and not being physically active. This suggests that the association relies on overall lifestyle patterns and eating habits, rather than sugars intake.
Sugars and Carbohydrates in the Diets of Individuals with Type 2 Diabetes
For people living with type 2 diabetes, the Diabetes Canada 2018 Clinical Practice Guidelines (12) suggests the following recommendations related to sugars and carbohydrates:
- Carbohydrates: About 45-60% of calories can come from carbohydrate, 15 to 20% from protein and 20 to 35% from fat so that eating plans can be tailored to treatment goals and personal preferences.
- Sugars: People with diabetes can eat sugars in moderation. In addition to naturally occurring sugars in fruits, vegetables and unsweetened dairy products, added sugars can be substituted for other carbohydrates as part of meals, up to 10% of total daily calories, as long as blood glucose levels are controlled and body weight is maintained. This is equivalent to 50 grams of added sugars per day for people with a daily energy intake of 2,000 calories.
- Glycemic Index: Choose low Glycemic Index (GI)/Glycemic Load (GL) foods more often (see table below).
Glycemic Index
The GI is a tool to measure the body's blood glucose response to consuming carbohydrate-containing foods.
Foods with a high GI result in a rapid increase in blood glucose compared to foods with a low GI. Recent studies show that consuming a low GI eating pattern more often improves blood glucose control, and reduces other cardiovascular and metabolic risk factors in people with diabetes (13).
However, it is important to note that the GI system does have some limits. For example,
- The GI of a single food may change when it is eaten with other foods as part of a meal or snack. For example, the GI of white bread is high when it is eaten alone, but if it’s eaten with a food like avocado, which has a low GI, the overall GI of the meal can be lower. High GI foods contain other important nutrients. For example, parsnips, winter squash and rutabaga have a high GI but are also rich in fibre, vitamins, and minerals.
- The GI of a food may vary depending on how it is processed or where it was grown. For example, converted rice has a low GI, basmati rice has a medium GI, and short-grain rice has a high GI as shown in the table below. Potatoes, when served cold (e.g. in salads), have a much lower GI value than hot potatoes.
Glycemic Load
The Glycemic Load (GL) is another measure of how food affects blood glucose levels. It not only accounts for the GI value, but also the amount of carbohydrate in the food. To calculate GL:
- GL = GI/100 x amount of carbohydrates (g) in a serving
For example,
- Watermelon has a high GI (80), but because each serving (120 g, ½ cup) contains very little carbohydrate (6 g), its effect on blood glucose is low (GL = 5).
- Spaghetti has a low GI (41), but because each serving contains a large amount of starch (40 g), its effect on blood glucose is medium (GL = 16).
Following a low GI/GL eating pattern can lead to small but important improvements in markers of blood glucose control (e.g. HbA1c), blood cholesterol, body weight, blood pressure, and inflammation, and may be useful as an add-on treatment to diabetes drugs or insulin in adults with type 2 diabetes (13).
Glycemic Index of Various Foods
| Low GI (<55) | Medium GI (55-70) | High GI (>70) | |
|---|---|---|---|
Grains and Starches |
All cereals provide energy, vitamins, and minerals. Whole grain and bran cereals also provide fibre. | ||
| Cereals | All Bran™, Steel Cut Oats, Oat Bran | Shredded Wheat™, Quick Oats | Rice Krispies™, Corn Flakes™, Bran Flakes™, Cheerios™, Instant Oats |
| Breads | Stone Ground Whole Wheat Bread, 12-Grain/Mixed Grain Bread, Pumpernickel Bread | Whole Wheat Bread, Rye Bread, Sourdough Bread | White Bread, White Bagel, Kaiser Roll |
| Grains/Pasta | Pasta (cooked al dente), Converted or Parboiled Rice | Basmati Rice, Brown Rice, Couscous | Instant Rice |
Fruits and Vegetables |
High GI vegetables such as parsnip, rutabaga, and winter squash, are also rich sources of vitamins, minerals and fibre. | ||
| Starchy Vegetables | Sweet potato, Green peas, Yams | Raw Carrots, Baked Potato with Skin, New Potato, Corn | Baked Potato without Skin, Mashed Potato, Parsnip, Rutabaga, Winter Squash |
| Fruit and Fruit Juices | Apple, Orange, Strawberries, Peach, Cherries, Grapes, Apple Juice, Orange Juice, Grapefruit Juice | Banana, Raisins, Apricots, Grape Juice, Cranberry Cocktail | Watermelon, Dried Dates |
Milk Products |
Milk products provide important minerals for bone health including calcium, phosphorus and magnesium. | ||
| Milk, Plain Yogurt, Sweetened Yogurt, Chocolate Milk | Sweetened Condensed Milk | ||
Legumes |
Legumes, including beans and lentils, are an excellent source of protein and fibre. | ||
| Lentils, Kidney Beans, Chickpeas, Baked Beans | |||
Sugars |
Maple syrup, brown sugar, honey, and white sugar (sucrose) are all mainly carbohydrates and provide the same number of calories (4 Calories per gram). | ||
| Fructose | Table Sugar (Sucrose), Brown Sugar, Honey | Glucose (GI = 100) | |
Source: International table of glycemic index and glycemic load values: Am J Clin Nutr 2002;76:5-56
For more information, additional resources include:
- Factsheet - Effect of Sugars on Metabolic Disease Risk Factors
- Factsheet - Frequently Asked Questions About Carbohydrates and Type 2 Diabetes
- Factsheet - Frequently Asked Questions: Sugars and Chronic Disease
- Clips on Sugars - Understanding the Glycemic Index
- Video - Sugar 101: Carbohydrates and Type 2 Diabetes
Recent news items include:
- January 2022 - New Fact Sheet: Effect of Sugars on Metabolic Disease Risk Factors
- September 2016 - A Closer Look at a Recent Debate on Sugars at the World Diabetes Congress
References
- Ekoe JE, Goldenberg R, Katz P. Diabetes Canada 2018 Clinical Practice Guidelines: Screening for Diabetes in Adults. Can J Diabetes. 2018;42(Suppl 1):S16-19.
- Prebtani APH, Bajaj HS, Goldenberg R, Mullan Y. Diabetes Canada 2018 Clinical Practice Guidelines: Reducing the Risk of Developing Diabetes. Can J Diabetes. 2018;42(Suppl 1):S20-26.
- World Health Organization. Diabetes Fact Sheet [Internet]. 2023 Apr 5 [cited 2024 Feb 26].
- Diabetes Canada. Healthy Eating Tips [Internet]. 2024 [cited 2024 Feb 26].
- European Food Safety Authority Panel on Nutrition, Novel Foods and Food Allergens, Turck D, Bohn T, Castenmiller J, de Henauw S, Hirsch-Ernst KI, et al. Scientific Opinion on the Tolerable Upper Intake Level for Dietary Sugars. 2022 p. e07074.
- Tsilas CS, de Souza RJ, Mejia SB, Mirrahimi A, Cozma AI, Jayalth VH, Ha V, Tawfik R, Di Buono M, Jenkins AL, Leiter LA, Wolever TMS, Beyene J, Khan T, Kenall CWC, Jenkins DJA, Sievenpiper JL. Relation of total sugars, fructose and sucrose with incident type 2 diabetes: a systematic review and meta-analysis of prospective cohort studies. CMAJ. 2017;189(20):E711-20.
- Choo VL, Viguiliouk E, Blanco Mejia S, Cozma AI, Khan TA, Ha V, Wolever TMS, Leiter LA, Vuksan V, Kendall CWC, de Souza RJ, Jenkins DJA, Sievenpiper JL. Food sources of fructose-containing sugars and glycaemic control: systematic review and meta-analysis of controlled intervention studies. BMJ. 2018 Nov 21;363:k4644.
- Rippe JM, Angelopoulos TJ. Added sugars and risk factors for obesity, diabetes and heart disease. Int J Obes (Lond). 2016 Mar;40 Suppl 1:S22-7.
- Khan T, Chen V, Lee D, Tayyiba M, Saleh A, Ahmed A, Au-Yeung F, Majia SB, Chiavaroli L, Malik V, Lieter L, Wolever T, Kendall C, Sievenpiper J. Important Food Sources of Sugars and Type 2 Diabetes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Can J Diabetes. 2022;46(7)S11-12.
- Imamura F, O’Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, Forouhi NG. Consumption of sugar-sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. Br J Sports Med. 2016;50(8):496–504.
- Lean ME, Te Morenga L. Sugar and Type 2 Diabetes. Br Med Bull. 2016 Dec;120(1):43-53.
- Sievenpiper JL, Chan CB, Dworatzek PD, Freeze C, Williams SL. Diabetes Canada 2018 Clinical Practice Guidelines: Nutrition Therapy. Can J Diabetes. 2018;42(Suppl 1):S64-79.
- Chiavaroli L, Lee D, Ahmed A, Cheung A, Khan TA, Mejia SB, Mirrahimi A, Jenkins DJA, Livesey G, Wolever TMS, Rahelic D, Kahleova H, Salas-Salvado J, Kendall CWC, Sievenpiper JL. Effect of low glycaemic index or load dietary patterns on glycaemic control and cardiometabolic risk factors in diabetes: systematic review and meta-analysis of randomised controlled trials. BMJ. 2021 Aug; 374:n1651.


